At a clinic in New Hampshire, cognitive behavioural therapy is used to treat chronic pain.Credit: Dartmouth Health
When Toby Moorsom was 19, he had a knee injury and, a few months later, a car accident. Following surgery to restore his mobility, he was prescribed strong pain medication. However, he wasn’t offered physiotherapy or rehabilitation, and there were no programmes accessible from his rural home. A few years later, he experienced gastric ulcers and low back pain; over time, the joint and gastrointestinal pain became constant. “In 26 years, I never had a period without pain,” says Moorsom.
Today, he teaches African studies at Carleton University in Ottawa. His pain journey is all too common, with repeated attempts to find relief through professional help and self-care. Finally, diagnoses of serious autoimmune conditions shed light on the cause of his pain. Although he has had surgery and takes non-opioid medication, much of his continuing pain management now involves non-invasive, non-pharmacological (NINP) therapies. Thanks to vigorous exercise (he has taken up surfing), physiotherapy, psychological therapy and dietary changes, his pain is much more manageable. “Today is a bad day — the pain is five out of ten,” he says. “But in a couple of days, I can have it down to a three. I don’t feel stressed by the pain level being high.”
Nature Outlook: Pain
NINP approaches have one enormous advantage. Most of them “have few or no harms related to routine use, unlike opioids”, says Andrea Skelly, a clinical epidemiologist in Kirkland, Washington. Moreover, she adds, “the benefits appear to be quite similar to the medications available”. Skelly was the lead author of a systematic review of NINP chronic pain therapies for the US Agency for Healthcare Research and Quality (AHRQ)1.
Pain specialists find that many people want to avoid drugs. “I’m increasingly hearing that patients don’t want to take any medication — opioid or non-opioid — because of side effects,” says Bruce Vrooman, a pain specialist at Dartmouth Hitchcock Medical Center in Lebanon, New Hampshire.
Research shows that NINP approaches are not only much safer but also effective2. Many NINP techniques have been studied in trials that are as rigorous as those used for drugs or surgery, including randomized controlled trials comparing NINP therapies with sham procedures, usual care and no treatment. Organizations that review research, such as the AHRQ in the United States and the National Institute for Health and Care Excellence (NICE) in the United Kingdom, have assessed the quality of NINP studies and the effectiveness of such therapies in improving an individual’s pain and ability to function.
Skelly says that although the strength of evidence for many NINP therapies is moderate or low, that’s true of drug therapies as well. At the same time, new therapies such as virtual reality (VR) hold promise, and some approaches are being offered remotely — available any time, anywhere — to reach more people. As a result of the mounting evidence, new modalities and avoidance of opioids, NINP therapies occupy a growing sector in pain treatment. Most importantly, “they can restore hope”, says Vrooman.
“The fear that comes from not being able to escape the pain is real,” says Matthew McGirt, a spinal neurosurgeon at Carolina NeuroSurgery and Spine Associates in Charlotte, North Carolina. “When patients can do something that they can control and that can actually work, it provides a mental health boost,” he adds. “There’s an optimism that is immediately seen in patients.”
Brain and body
Many NINP therapies, such as acupuncture and t’ai chi, have been used for centuries; others, such as cognitive behavioural therapy, for decades. However, it remains unclear how they influence chronic pain.
A prevalent view is that injury or inflammation heightens the sensitivity of the central nervous system, which includes the spinal cord and brain. Clifford Woolf, a neurobiologist at Harvard Medical School in Boston, Massachusetts, first demonstrated this ‘central sensitization’ in animals more than 40 years ago3. When he applied noxious stimuli to animals, the affected neurons initially had small receptor fields and therefore high thresholds for pain. As he repeatedly applied the stimuli, the receptor fields became larger and the pain thresholds lower.
“That was the breakthrough,” Woolf says. Previously, it was thought that pain was a consequence of damage to the peripheral nervous system — the nerves in the body that carry messages to and from the central nervous system. Woolf found, however, that the neural circuits themselves could change their properties and function — in both the peripheral and central nervous system. “There is pathological change in the nervous system itself,” he says.
When the sensory endings in the body that detect possible tissue damage, known as nociceptors, are activated even briefly, the immune system responds. Proteins such as cytokines and chemokines, which are involved in the immune response, act on neurons in the peripheral nervous system, making them more sensitive. In the spinal cord, microglia — immune cells often called the guardians of the brain — are also activated and contribute to sensitization in the central nervous system. There is also heightened sensitivity and synaptic function in the dorsal horn of the spinal cord, in which sensory signals from the periphery enter the central nervous system. Circuits that inhibit pain might be lost as well, Woolf explains. Many pain researchers think that the physiological changes during peripheral and central sensitization mark the transition from acute to chronic pain4.
Originally, Woolf says, it was thought that central sensitization occurred solely in the spinal cord. However, many of the inhibitory circuits linked to central sensitization descend from the brain, and Woolf thinks that NINP therapies can reduce pain by acting on circuits in the brain. “Whether it’s exercise, acupuncture or deep-brain stimulation, it can activate inhibitory circuits that can reduce the heightened excitability.”
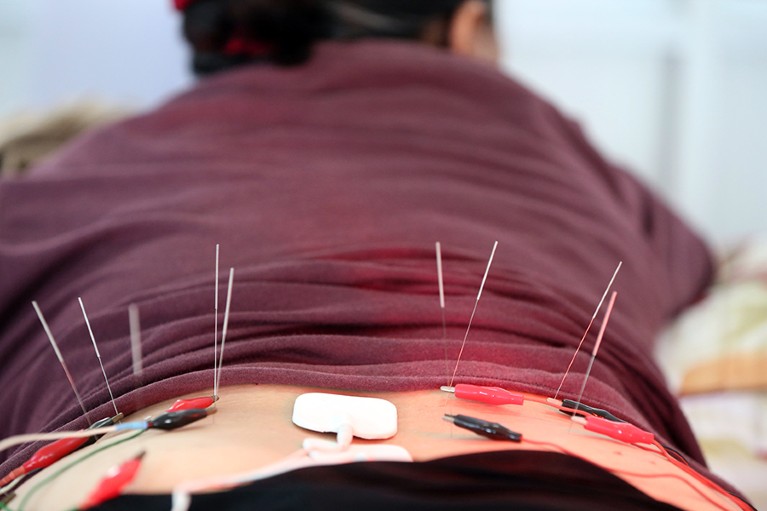
Acupuncture can be used to help manage chronic pain.Credit:BSIP/UIG via Getty
Some researchers are sceptical of this view of chronic pain. “This idea that there’s acute pain and that it transitions to chronic pain is controversial,” says Jeffrey Mogil, who studies the neurology of pain at McGill University in Montreal, Canada. “There is pain — sometimes it resolves and sometimes it doesn’t.”
“All chronic pain involves some kind of injury, whether we can see it or not.” He says research over the past 20 years shows that chronic pain involves not only the nervous system but also the immune system, which fails to repair the injury: “it didn’t do what it was supposed to do”. Furthermore, he says, many people who experience chronic pain do not have central sensitization.
Mogil agrees with Skelly that drug therapies have variable effectiveness. Between one in three and one in eight people get significant relief from a treatment, with the former considered a good result and the latter considered poor. But he says that non-pharmacological approaches are often worse, with the treatment working for only around one in 12 people. “That’s just terrible,” he says.
Assessing the alternatives
Evidence for many NINP therapies comes from clinical trials comparing them with other approaches. For some therapies there is a strong evidence base with dozens of studies, whereas other approaches lack research. Several public organizations have assessed existing evidence to help guide practitioners and individuals experiencing pain.
Exercise is recommended for a wide range of chronic pain conditions, on the basis of dozens of studies comparing it with usual care, attention control, placebo, sham treatment and no treatment. The AHRQ review finds that exercise improves function in people with low back pain, osteoarthritis in the knee or hip and fibromyalgia — a condition that causes pain all over the body. The UK NICE guideline on the assessment and management of chronic pain says that physicians should prescribe exercise to people for many types of chronic primary pain, on the basis of data from studies mainly on fibromyalgia and neck pain5.
Cathy Stannard, a consultant in pain medicine, helped to develop the NICE guideline. She works at the UK’s National Health Service Gloucestershire Integrated Care Board in Gloucester, UK. Stannard says evidence shows that exercise classes led by instructors have a greater effect on pain than exercise in one-on-one sessions guided by physiotherapists — possibly because exercise classes offer peer-to-peer support, motivation to attend and continue, as well as social benefits. Exercise is also “very, very cost-effective”, Stannard says.
Another approach shown to help relieve chronic pain is cognitive behavioural therapy (CBT), which involves identifying and changing negative thought patterns. A team led by Benjamin Rosser, a psychologist at Liverpool John Moores University, UK, reviewed 25 studies of CBT, which was delivered remotely, involving almost 4,000 participants6. Rosser’s group found that CBT relieved pain intensity compared with usual care. Indeed, 23% of participants receiving CBT in the pooled studies achieved a 30% improvement in pain; among people receiving usual care, only 11% had that high a level of pain reduction.
The AHRQ review found that CBT improved function and pain levels in low back pain, fibromyalgia and knee osteoarthritis, compared with usual care. The NICE guideline recommends CBT to improve quality of life.
CBT can be offered remotely, reaching more people than conventional, in-person therapy. Rosser and his colleagues reviewed studies of CBT and another form of behaviour therapy called acceptance and commitment therapy offered over the Internet6. Such programmes can reach people who live far from clinics and centres. Studies show that remote CBT, defined as less than 30% of therapy time involving contact with another person, probably lessens pain and might slightly reduce disability.
Rosser says these results are similar to what was found in a review of studies of conventional, in-person CBT7. But, whereas in-person CBT has been shown to have long-lasting results, the long-term effect of remote CBT has not yet been sufficiently studied, he says.
Views on the value of CBT — whether in-person or remote — range widely. Mogil counts himself as a sceptic. “CBT does not work enough to start seriously interrogating it,” he says. But many other pain specialists see at least some value in the practice. Rosser says that CBT improves chronic pain by addressing pain’s multi-faceted effects on people’s lives. “The impact of pain is not just physical, it’s psychological, and it’s to do with a person’s behaviour as well. The tendency for us to develop unhelpful patterns of thoughts and behaviours can exacerbate the situation we find ourselves in. Being able to identify these unhelpful patterns and find more helpful ways of considering our experience helps us improve our quality of life.”
Vrooman, similarly, finds CBT effective for some people, and his clinic offers a multidisciplinary functional restoration programme that includes group CBT. Moorsom says his pain experience is worsened by any psychological pain, creating a “negative feedback loop”. Psychotherapy is an important part of how he manages pain, he says. And the AHRQ review and NICE guideline also present evidence for other holistic practices, including acupuncture, yoga and t’ai chi.
Virtually relieved of pain
The latest NINP therapy is VR, in which mindfulness interventions, exercise games and visual illusions are being tested to treat chronic pain. For example, a person in pain puts on a headset and is immediately immersed in a new environment — they can follow a meditation beside a misty lake, watch waves crash on a seashore at night or hang-glide over a landscape. Or they can guide an avatar through exercises, using their healthy arm to move the avatar’s counterpart to their injured arm, for example.
Research has shown that such systems provide significant improvements in pain and function8: the pooled effect size — a measurement that can be used to determine the effectiveness of a treatment — for pain relief is 1.60, which is considered strong. Lisa Goudman, a pain researcher at Vrije Universiteit Brussel in Belgium, co-authored a review of 41 research papers on this approach8. Her conclusion: “VR works for chronic pain.”

Virtual-reality therapy can help to reduce pain intensity.Credit: Karuna Labs Inc.
One application developed for chronic pain combines CBT and VR9. Called Vx Therapy, the proprietary service was developed by Harvard Medtech, a company that develops technology-enabled health services based in Las Vegas, Nevada. McGirt is a medical adviser for the firm and has studied the approach in people with chronic neck and low back pain. He says that the VR component “lets anyone escape where they are. At 2 a.m., they can pop on the VR headset, and they go to a different place”. One study showed that enabling people to immerse themselves in a serene virtual environment lowered pain and anxiety, with self-reported pain falling a few points on a scale of 0–10 during a VR session9.
In another VR therapy, people control an avatar of their own body using hand controllers, and it can help them to move without fear of pain. This ‘virtual embodiment training’ builds on research in which people with phantom limb pain can improve it by using mirrors to create an image of their missing limb, says Lincoln Nguyen, the chief executive of Karuna Labs in Ione, California, which developed the system. A pilot study of this training has shown improvements in pain intensity, disability and feelings of helplessness10.
It’s not clear exactly how a VR experience helps to dampen pain. Goudman says it might be through distraction, because VR competes with pain for the person’s attention. McGirt offers a different perspective. He thinks that VR helps to counteract central sensitization through the inhibitory circuits in the brain. “It takes the centres of the brain that are meant to suppress pain, and trains them,” he says.
Part of the VR effect is probably a consequence of neuroplasticity — the ability of neural networks to change through growth and reorganization. “The brain has the ability to protect you so you don’t further injure yourself,” says Nguyen. “In chronic pain, the signal is too good, even in the absence of tissue damage.” VR, he argues, essentially gives people the confidence to change their behaviour and learn that it won’t hurt. Nguyen says people often fear moving an injured limb, but making such motions through VR dampens the threat response, allowing the person to move more, with less pain, in real life.
More from Nature Outlooks
For many people experiencing chronic pain, picking one or multiple NINP approaches from a menu helps more than any specific technique. “Whether it’s t’ai chi, swimming, pilates or yoga, it should be something you want to do and enjoy, and at a pace that’s suitable for you,” says Stannard. Vrooman and a multidisciplinary team offer a programme at their clinic that includes several NINP approaches — education, exercise and group and individual discussions. Vrooman says that the programme usually meets or exceeds people’s goals to be able to return to activities in their daily lives, work and recreation.
Using several techniques recommended by professionals and from his own research, Moorsom has built his own pain-management programme. And he is a one-person study of a unique modality — surfing. He took up the sport while doing a fellowship in Jamaica, and it quickly became one of the ways he manages pain.
“In the seconds that you are on a wave, you are not feeling pain. You’re not thinking about the past or the future. You’re in the present, and you have respite.”
Source link